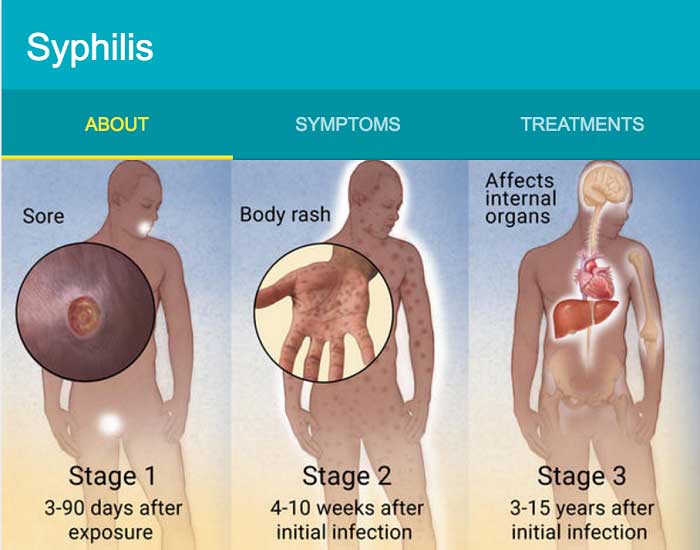
Syphilis is a sexually transmitted disease (STD) caused by the bacterium Treponema pallidum. It can cause serious symptoms, even death, if not treated. The symptoms of syphilis occur in three distinct (active) stages. The primary (first) stage is usually characterized by round, painless sores localized to the initial site of infection (genitals, anus, mouth) that last for about 3-6 weeks. The sores heal on their own, but if not treated, the disease moves into the secondary stage. This stage is characterized by a more widespread rash and/or mucous membrane lesions. The rash can occur in different locations on the body, although it classically appears on the palms of the hands and bottoms of the feet. It may be so faint it goes unnoticed, or it can look very similar to rashes from other diseases. There are other symptoms in addition to the rash: fever, swollen lymph glands, sore throat, patchy hair loss, headaches, weight loss, muscle aches, and fatigue. These symptoms also go away on their own, but without treatment, the disease can progress to the tertiary stage. After the secondary stage outbreak, syphilis will transition to the latent stage. This means that there are no visible signs or symptoms of the disease, but the person is still infected. In some cases, syphilis progresses to the tertiary stage, which can affect multiple organ systems and be potentially fatal (symptoms vary depending on organ system affected). Syphilis is known as “The Great Pretender” because its symptoms can be mistaken for several other diseases. Transmission occurs through direct contact with “syphilitic sores,” aka “chancres,” or from mother to unborn child (congenital syphilis).

https://cmr.asm.org/content/18/1/205/F1
Syphilis is treated with antibiotics, specifically Benzathine penicillin G, administered intramuscularly. There are alternative antibiotics for those who cannot take penicillin, such as doxycycline and tetracycline. Treatment with antibiotics will prevent progression of the disease, but may not be able to reverse damage caused prior to treatment. However, proper treatment will prevent the disease from recurring (from the intial infection — it does NOT prevent a second infection of syphilis). There are certain groups of people that the CDC recommends routinely testing for syphilis due to increased risk. Pregnant women, for example, should be screened due to the effects of congenital syphilis. In up to 40% of cases of (untreated) infected mothers, the infant dies. In cases where the baby survives to term, but remains untreated, the baby could develop seizures, become developmentally delayed, or die within a few weeks. Penicillin is extremely effective at preventing mother-to-child transmission. Other high-risk groups include men who have sex with men (MSM), who make up the majority of recent cases of syphilis. In 2018, there were over 35,000 reported cases of primary and secondary syphilis, and 64% of those were among MSM. This is likely due to the greater prevalence of high-risk sexual behaviors in this community: greater numbers of sexual partners, higher rates of condom-less sex, type of intercourse, etc.
Syphilis, among other STDs, is on the rise in the U.S. The CDC made a press release in October 2019 discussing the increase in syphilis cases, particularly with its effect on the newborn population. From 2017 to 2018, the number of primary and secondary syphilis cases increased 14% to more than 35,000 cases, “the highest number reported since 1991.” This corresponded with a 40% increase in cases of congenital syphilis (to more than 1300 cases). Granted, part of the reason for the large percentage increases is due to the relatively small number of cases (e.g. going from 1 to 2 cases per year would be a 100% increase, but going from 100 to 101 would only be a 1% increase), but it is still concerning that the number of cases is increasing for a disease that could be eliminated entirely.
There is interesting research on the reasons for this upward trend in syphilis cases. Suggested explanations include: increases in risky sexual behavior due to dating apps/online dating, perception of reduced risk of HIV due to advances in HIV/AIDS treatments (e.g. chronic condition rather than a death sentence, preventive medications such as pre-exposure prophylaxis), and increased drug use, which increases likelihood of risky sexual behaviors. There have also been decreases in funding for public health initiatives that educate and provide sexual health services to the community. This decreases the number of clinics and screening services available to at-risk populations. Also, considering that MSM are disproportionately affected by syphilis, it is important to note that anal intercourse also increases risk of transmission (relative to vaginal intercourse) due to the higher probability of abrasions and the highly vascularized nature of the rectum (increased chance of exposure of the bloodstream to the pathogen).
The only sure-fire way to avoid syphilis and other STDs is abstinence, but there are other precautions that people can take to prevent infection. Many people don’t realize that condoms are useful for more than just preventing pregnancy, and this is important to know in populations who don’t think that they need to use condoms, because they already avoid vaginal sex. When people in populations such as MSM (who do not need to worry about pregnancy) have unprotected sex, they are putting themselves at higher risk for contracting STDs such as syphilis. Condoms provide a physical barrier that prevents transmission of STDs through direct contact. [Side note: this is NOT 100% effective, especially if syphilis sores are present in areas not covered by the condom (duh)]. Another way to reduce transmission is to practice mutual monogamy. Obviously, the fewer sexual partners one has (and the fewer partners their partner has), the less likely they are to contract an STD. Syphilis is easily treatable, but also VERY preventable through safe sexual practices. Through the combination of treating current cases and preventing new ones, syphilis could be eliminated.